CAR T-cell Therapy
CAR T-cell therapy allows us to engineer your own cells to fight your cancer from within. Our program was one of the first to be certified in CAR T-cell therapy for adults with recurrent or persistent diffuse large B-cell lymphoma (DLBCL), a common type of non-Hodgkin lymphoma, and children and young adults (at NewYork-Presbyterian Morgan Stanley Children’s Hospital) with recurrent or persistent acute lymphoblastic leukemia (ALL).
Our team’s expertise and skill, along with access to top specialists from all areas of medicine in one medical center, make the HICCC the place to receive this potentially lifesaving treatment.
What is CAR T-cell therapy?
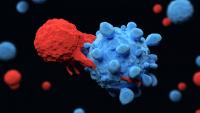
CAR T-cell therapy is a type of immunotherapy that trains the immune system to attack cancer with a patient’s own T-cells, a type of white blood cell. CAR stands for "chimeric antigen receptor." In CAR T-cell therapy, our specialized teams collect T cells from the patient and engineer them to express the CAR, turning these cells into ‘serial killers’ that seek and destroy cancer cells.
CAR-T cell therapy is a powerful new tool for clinicians and researchers at the HICCC in the fight against cancer.
Our approach and expertise
You'll have your own team of experts. In addition to your stellar team of physicians, nurses, and nurse practitioners with expertise in cancer care, you will have access to a wide range of other specialists that will help you through your CAR T-cell treatment process. Our bone marrow and stem cell transplantation programs are accredited by the Foundation for the Accreditation of Cellular Therapy (FACT), and our team performs a large number of transplants and cell therapy procedures each year.
Experience and safety go hand-in-hand. Our CAR T-cell team has years of experience administering this treatment and are leaders in the field. They know how to give CAR T cells safely and manage any complications or side effects that may arise. They also have a great deal of experience caring for patients with multiple health problems and complex medical needs and work closely with teams in the intensive care unit and neurology services to provide optimal care for CAR T patients. Our team also leads research into continuously improving the safety and effectiveness of CAR T-cell therapy and minimizing side effects so you can focus on healing.
We're leading the way with new treatments. CAR T-cell therapy is a revolutionary way to treat cancer, and our physicians and researchers are dedicated to advancing the field and finding new ways to help people with other types of cancer and other diseases. Our researchers and physicians are leading clinical trials for CAR T-cell and other cell therapies so that we can offer this revolutionary treatment to patients with many different cancer types.
Learn More About Clinical Trials at the HICCC
NewYork-Presbyterian/Columbia has an onsite, in-house Cellular Immunotherapy Laboratory, where our scientists can develop our own cellular therapies quickly, efficiently, and effectively, based on the newest research.
We give you dedicated, compassionate care. CAR T-cell therapy is a very intensive treatment that requires dedicated care. Jump-starting the immune system with CAR T-cell therapy can cause side effects that signify that the treatment is working, but which also require close monitoring and management. As one of the top five best hospitals in the United States, NewYork-Presbyterian has specialists and subspecialists from every area of medicine to care for people throughout their CAR T-cell therapy.
Most complications of CAR T-cell therapy occur within the first four weeks after treatment. If receiving this treatment at NewYork-Presbyterian/Columbia University Irving Medical Center means you are far from home, we can assist you and your family with accommodations closer to the hospital.
Is CAR T-cell therapy right for me?
Currently, CAR T-cell therapy is FDA-approved as standard therapy for some adults with non-Hodgkin lymphoma that has relapsed or has not responded to other treatments (refractory), and for young patients (25 or under) with relapsed or refractory B-cell acute lymphoblastic leukemia.
These revolutionary treatments are offered at only a few institutions across the country. We offer both these treatments in our specialized centers at NewYork-Prebsyterian/Columbia University Irving Medical Center and Morgan Stanley Children’s Hospital, for young patients.
In addition to these standard of care therapies, our researchers and physicians are finding new ways to offer CAR T-cell therapies for many different cancer types through leading innovative clinical trials.
For more information about CAR T-cell therapy at NewYork-Presbyterian/Columbia or to schedule a consultation for you or a loved one, call 212-305-4417 or email BMTCOORD@nyp.org.
What are some of the possible side effects of CAR T-cell therapy?
Cytokine release syndrome: CAR T-cells are very feisty which makes them highly effective against cancer, but also capable of causing side effects. When CAR T-cells enter the body, they cause a release of cytokines, proteins that recruit other parts of the immune system to attack cancer. Sometimes this response is too aggressive, causing cytokine release syndrome (CRS). Symptoms of CRS may resemble a bad flu, including fever, chills and fatigue and in severe cases also low blood pressure and difficulty breathing.
Neurologic symptoms: Some patients also experience side effects involving the nervous system, including confusion, difficulty to find words or understand questions. The causes of these symptoms are not well understood, but the symptoms are treatable and generally subside within a few days or in extreme cases, weeks.
Patients will be observed in the hospital for at least one week after their CAR T-cell infusion so that our specialized care team can closely monitor them and manage any side effects that may arise. Our transplant and cell therapy team has assembled a multidisciplinary team that includes experts in intensive care and neurology and part of their research is dedicated to understanding the causes of cytokine release syndrome and neurotoxicity, and developing ways to prevent or decrease these side effects.
Currently, any patient undergoing CAR T-cell therapy at Columbia is seen by a neuro-immunologist prior to admission and undergoes a neurological assessment and brain MRI to obtain baseline information against which any changes can be compared following therapy. If a patient develops a severe neurological symptom, our highly experienced neurological ICU is immediately available.
To date, the team’s experience in managing CAR T-cell side effects has been very positive, allowing the team to treat safely all types of patients, including patients with diseases that are highly refractory to standard treatments, as well as elderly individuals and those with underlying medical conditions.