New Research Reveals Promising Drug Target in Recurrent Lung Cancer
A new study has identified a novel combination therapy that has the potential to stop metastatic tumor growth in lung cancer patients whose cancer has relapsed in the brain following targeted therapy. Brain metastasis is a debilitating complication seen in lung cancer patients that impair daily functioning, cognitive decline, and accelerated death.
Mutations in the epidermal growth factor receptor (EGFR) gene occur in up to 50% of lung cancer patients worldwide. Targeted EGFR therapies have transformed the treatment landscape for this subtype of lung cancer, resulting in more patients’ prolonged survival. While this targeted therapy has been effective for many patients, killing tumor growth and with little side effects, there is a population of patients who eventually develop lethal metastatic cancer, sometimes several months to years following remission.
In a paper published in Cancer Discovery, Columbia University researchers uncovered a signaling pathway in EGFR-mutant lung cancer responsible for driving recurrence and metastases, spreading to the brain.
Specifically, the researchers investigated disease recurrence after treatment with osimertinib, a highly successful targeted therapy for EGFR-positive lung cancer. Their work revealed that the signaling pathway, called S100A9-ALDH1A1-RA, is responsible for driving osimertinib-refractory lethal brain relapse, and identified an inhibitor to shut down that pathway and prevent cancer progression in preclinical models.
“We were very interested in learning why patients who were successfully treated with osimertinib suddenly come back, sometimes years later, with a more lethal presentation of the disease,” says Swarnali Acharyya, PhD, Herbert Irving Assistant Professor of Pathology and Cell Biology in the Institute for Cancer Genetics (ICG) at the Vagelos College of Physicians and Surgeons (VP&S), and the study’s principal investigator and lead author.
“We found that some cancer cells, after osimertinib treatment, hide in the brain and are responsible for disease recurrence. These metastatic cancer cells no longer die from osimertinib and have learnt new tricks to thrive in the brain,” says Dr. Acharyya, also a member of the Tumor Biology and Microenvironement program at the Herbert Irving Comprehensive Cancer Center (HICCC). “If there is a way to block the molecular pathway driving relapse, we can significantly prolong survival for this lung cancer subtype.”
Shutting down the lethal pathway
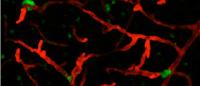
Dr. Acharyya and her group developed mouse models that closely resemble the metastatic progression observed in human patients treated with osimertinib. They generated long-term in vivo treatment models using osimertinib-sensitive EGFR-mutant human lung cancer cell lines that metastasize to distant organs, including the brain. These mice showed remarkable initial responses to osimertinib that corresponded with human patients, with a long window of disease-free survival followed by metastatic relapse. These treatment models, which have been missing in the field, say the researchers, will be useful for the cancer research community to study residual disease and relapse mechanisms in different metastatic organs in response to osimertinib.
To identify the cellular drivers of relapse using these models, the researchers conducted proteomic and transcriptomic profiling— analysis of changes in the genes being read by the cellular machinery and the proteins that are produced—in relapsed brain metastatic cells. They discovered that the mice with recurrent disease after treatment with osimertinib expressed higher levels of the protein, S100A9 in brain metastatic cells, and were the ones that suffered from aggressive recurrent disease, an observation that was confirmed in patients in this study.
The researchers then worked to identify an agent that could block this pathway to keep recurrence at bay. They found that the retinoic acid (RA) pathway antagonist AGN194310, a drug that has growth-inhibitor effects in prostate cancer cells, is very effective in blocking brain metastasis in lung cancer models. In this study, when mice are treated with this drug, in combination with osimertinib, it kills residual cancer cells hiding in the brain.
“After a period of striking response with osimertinib treatment, when tumors relapse in patients, it is very challenging to eliminate them,” says the study’s first and co-corresponding author, Anup Kumar Biswas, PhD, an associate research scientist at ICG. “If we can unlock the underlying mechanism responsible for relapse in these patients, then we can potentially save a lot more lives suffering from this type of lung cancer.”
Putting an end to recurrent disease
Lung cancer is the leading cause of cancer death among both men and women in the U.S., making up almost 25% of all cancer deaths. This year, an estimated 237,000 new cases of lung cancer will be diagnosed.
“We want therapeutic strategies to intervene early, not giving the cancer a chance to re-emerge,” says Dr. Acharyya.
“It is a continuous challenge in the field—not knowing where the minimal residual disease is hiding and when it might start to re-grow. By developing these models to study therapy response and relapse,” she says, “we are able to better understand other pathways that might also be active in these cancer cells evading therapy and identify new drugs to block their growth. It is promising that the new combination treatment (osimertinib and RA antagonists) in preclinical studies can significantly reduce minimal residual disease in the brain.”
The researchers, who collaborated closely with clinical colleagues at the HICCC and Memorial Sloan Kettering Cancer Center, plan next to translate these findings in patients. They are also testing new drug combinations that can block the S100A9-ALDH1A1-RA pathway and prevent brain relapse.
More information:
The paper is titled “Targeting S100A9-ALDH1A1-retinoic acid signaling to suppress brain relapse in EGFR-mutant lung cancer”.
All authors (at Columbia University unless noted otherwise): Anup Kumar Biswas, Seoyoung Han, Yifan Tai, Wanchao Ma, Courteny Coker, S. Aidan Quinn (Dana-Farber/Harvard Cancer Center), Ahmad Rushdi Shakri (University of South Florida), Timothy James Zhong, Hanna Scholze (Albert Einstein College of Medicine), Galina G. Lagos (Brown University), Angeliki Mela, Katia Manova-Todorova (Memorial Sloan Kettering Cancer Center), Elisa de Stanchina (Memorial Sloan Kettering Cancer Center), Adolfo A. Ferrando, Cathy Mendelsohn, Peter Canoll, Helena A. Yu (Memorial Sloan Kettering Cancer Center), Paul K. Paik (Memorial Sloan Kettering Cancer Center), Anjali Saqi, Catherine A. Shu, Mark G. Kris (Memorial Sloan Kettering Cancer Center), Joan Massague (Memorial Sloan Kettering Cancer Center), and Swarnali Acharyya.